Fatigue: A Common Companion to Hot Flushes in Perimenopause
October 20, 2024

What Causes Hot Flashes and Fatigue?
Hot flashes result from hormonal fluctuations, particularly decreasing estrogen levels, which affect the hypothalamus—the part of the brain responsible for regulating body temperature. These sudden temperature surges can disrupt sleep, leaving women feeling exhausted and drained. This often leads to additional symptoms like hot flashes and fatigue headache, nausea, body aches, brain fog, and even dizziness.
Fatigue, on the other hand, can stem from various factors, including hormonal imbalances, poor sleep quality, and the physical toll of frequent hot flashes. For some women, symptoms such as hot flashes and fatigue shortness of breath or nausea dizziness can further exacerbate feelings of tiredness. Emotional exhaustion and loss of appetite may also play a role in creating a cycle that’s hard to break.
What Causes Menopause Fatigue?
1. Hormonal Changes
As menopause approaches, the decline in estrogen and progesterone affects several key processes in the body, including energy regulation and sleep. Estrogen helps regulate serotonin, a neurotransmitter that promotes feelings of happiness and relaxation. When estrogen levels drop, serotonin levels may also decline, leading to mood swings, irritability, and difficulty falling asleep. Progesterone, often called the body’s natural “calming hormone,” also diminishes during menopause. This can lead to increased anxiety, making it harder to relax or achieve restful sleep. The combination of low estrogen and progesterone creates a cascade of effects that contribute to fatigue.
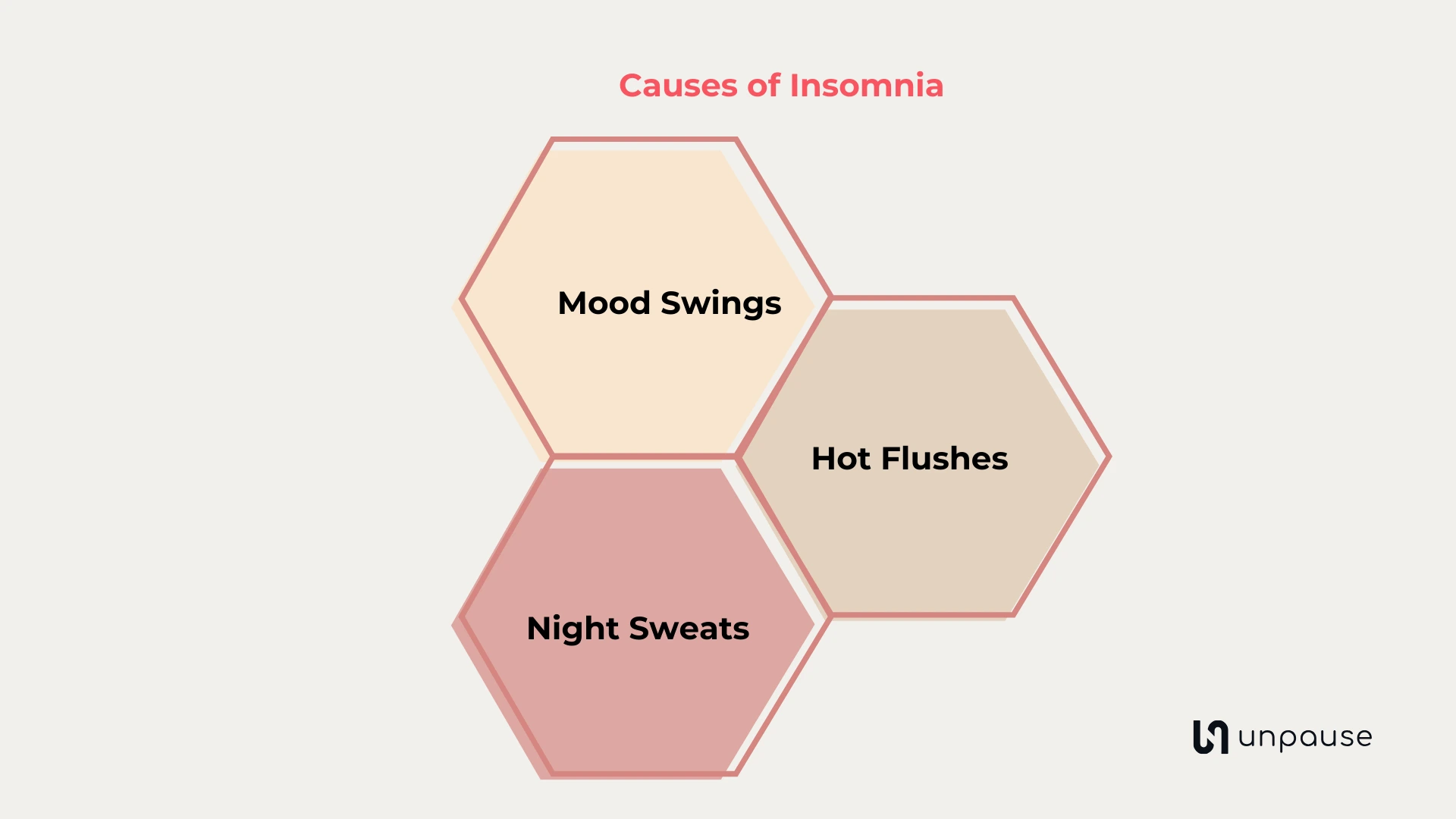
2. Sleep Disruptions
One of the most common complaints during menopause is poor sleep quality. Hot Flushes and night sweats can wake women multiple times during the night, preventing them from entering deep, restorative sleep cycles. Additionally, the hormonal changes associated with menopause can increase the risk of developing sleep apnea—a condition in which breathing temporarily stops and starts during sleep. Sleep disturbances often create a vicious cycle: the less you sleep, the more tired and irritable you feel, which further impacts your ability to rest.
3. Vasomotor Symptoms (VMS)
VMS such as Hot Flushes can directly trigger wakefulness, even without obvious sweating episodes. The brain’s thermoregulatory center is sensitive to these changes, causing sudden awakenings that disrupt the natural sleep-wake cycle.
4. Emotional and Psychological Factors
Menopause is a time of significant life transition, and many women experience heightened stress, anxiety, or depression during this period. Emotional distress can further exacerbate fatigue, creating a feedback loop that impacts both mental and physical health. How to Manage Menopause Fatigue
The good news is that menopause fatigue can be managed effectively through a combination of lifestyle adjustments, dietary changes, and medical therapies. Below are some evidence-based strategies to help alleviate exhaustion and restore energy:
1. Improve Your Diet
Nutrition plays a vital role in managing menopause symptoms, including fatigue. Here are some dietary tips:
Include soy-rich foods: Foods like tofu, tempeh, and soy milk contain phytoestrogens—plant-based compounds that mimic estrogen and may help balance hormones.
Eat magnesium-rich foods: Spinach, nuts, seeds, and whole grains are excellent sources of magnesium, which can help regulate sleep and support energy production.
Limit sugar and caffeine: While these can provide temporary energy boosts, they often lead to crashes that worsen fatigue over time. Stay hydrated: Dehydration can amplify feelings of tiredness, so aim for at least 8–10 glasses of water daily.
2. Make Lifestyle Adjustments
Stay active: Regular exercise, such as walking, yoga, or swimming, can improve energy levels and enhance sleep quality. Aim for at least 30 minutes of moderate activity most days of the week.
Prioritize sleep hygiene: Develop a bedtime routine that includes relaxing activities like reading or meditating. Keep your bedroom cool, dark, and free of electronic distractions.
Wear breathable clothing: Lightweight fabrics, especially at night, can reduce discomfort from Hot Flushes and night sweats.
3. Explore Medical and Alternative Therapies
Hormone Replacement Therapy (HRT): HRT can be highly effective in managing menopause symptoms, including fatigue. Discuss the risks and benefits with your healthcare provider to determine if it’s right for you.
Medications: Certain antidepressants, such as serotonin reuptake inhibitors (SSRIs), may help alleviate both mood issues and sleep disturbances.
Acupuncture: Many women find that acupuncture provides relief from sleep problems, fatigue, and even Hot Flushes. Oral contraceptives: Birth control pills may help regulate hormonal fluctuations during the transition to menopause.
4. Manage Stress and Emotions
Practice mindfulness: Techniques like meditation, deep breathing, and journaling can help reduce stress and improve emotional resilience.
Seek support: Talking to friends, joining menopause support groups, or consulting a therapist can provide valuable emotional support during this transition.
Causes of Perimenopause Fatigue
- Hormonal Imbalances: The decrease in estrogen and progesterone impacts sleep quality, energy levels, and mood.
- Sleep Disturbances: Night sweats, hot flashes, or anxiety can lead to insomnia or fragmented sleep.
- Stress and Emotional Strain: Mood swings or anxiety during perimenopause can increase feelings of mental and physical exhaustion.
- Nutritional Deficiencies: Decreased absorption of certain nutrients like iron, magnesium, or vitamin D can exacerbate fatigue.
- Lifestyle Factors: Lack of exercise, poor diet, or overcommitting can contribute to energy drain.
Symptoms of Perimenopause Fatigue
- Difficulty waking up even after a full night's rest
- Low energy throughout the day
- Brain fog or difficulty concentrating
- Irritability or mood swings due to exhaustion
- Muscle weakness or body aches
6 best ways to Manage Perimenopause Fatigue
1. Prioritize Sleep Hygiene
- Stick to consistent sleep and wake times.
- Create a calm, cool sleep environment.
- Use moisture-wicking sheets or cooling pillows to manage night sweats.
- Avoid screen time, caffeine, and alcohol before bed.
2. Balance Your Diet
- Include foods rich in magnesium, iron, and vitamin D.
- Stay hydrated to support overall energy levels.
- Eat phytoestrogen-rich foods like soy and flaxseeds to support hormone balance.
3. Exercise Regularly
- Gentle exercises like yoga or walking can improve energy levels and mood.
- Avoid intense workouts late at night to prevent sleep disruption.
4. Reduce Stress
- Practice mindfulness, meditation, or breathing exercises.
- Consider journaling or counseling to manage emotional strain.
5. Explore Medical Options
- Speak to a healthcare provider about hormone replacement therapy (HRT) or natural supplements like magnesium or melatonin.
6. Listen to Your Body
- Don’t overcommit; rest when needed.
- Break tasks into smaller, manageable steps.
Can Low Estrogen Cause Fatigue?
Yes, low estrogen levels are a common culprit behind fatigue, particularly during menopause or perimenopause. This hormonal change not only triggers hot flashes but can also contribute to tiredness, brain fog, and body aches, making everyday tasks feel overwhelming.
How Hot Flashes Affect Energy Levels
Hot flashes can disrupt sleep patterns, leading to insomnia or fragmented rest. Waking up repeatedly due to night sweats—a nocturnal form of hot flashes—can result in insufficient restorative sleep, leaving the body unable to recharge. This sleep deficit builds over time, contributing to chronic fatigue and impairing mental focus. Additionally, symptoms like hot flashes and fatigue and weight gain or dizziness further impact energy levels, creating a compounded challenge.
What Will Stop Hot Flashes?
While there is no one-size-fits-all solution, several approaches can help reduce the frequency and severity of hot flashes, thereby alleviating fatigue:
- Hormone Replacement Therapy (HRT): Consult a healthcare provider to determine if HRT is a suitable option.
- Lifestyle Changes: Regular exercise, a healthy diet, and stress management techniques can help manage symptoms.
- Natural Remedies: Supplements like black cohosh or evening primrose oil may provide relief for some women.
Breaking the Cycle: Strategies for Managing Hot Flashes and Fatigue
While hot flashes and fatigue can feel overwhelming, several effective strategies can help alleviate their impact:
1. Optimize Sleep Hygiene
- Stick to a consistent bedtime and wake-up schedule.
- Create a cool, comfortable sleeping environment.
- Use moisture-wicking sheets or a cooling pillow to manage night sweats.
- Avoid caffeine, alcohol, and heavy meals before bedtime.
2. Adopt a Balanced Diet
- Focus on nutrient-rich foods, such as fruits, vegetables, lean proteins, and whole grains.
- Include foods high in phytoestrogens (like soy, flaxseeds, and lentils) to help balance hormones.
- Stay hydrated to support overall energy levels.
3. Incorporate Regular Exercise
- Engage in moderate activities like walking, yoga, or swimming to boost energy and reduce stress.
- Exercise can also improve sleep quality, helping to counteract fatigue.
4. Manage Stress Levels
- Practice mindfulness techniques such as meditation or deep breathing to stay grounded.
- Consider journaling or talking to a trusted friend to process emotions.
5. Explore Medical Options
- Consult a healthcare provider about hormone replacement therapy (HRT) or non-hormonal treatments that may alleviate symptoms.
- Ask about supplements such as magnesium or melatonin to support sleep and energy.
6. Listen to Your Body
- Prioritize rest when you’re feeling overwhelmed.
- Break tasks into manageable steps and avoid overcommitting.
Hot Flashes and Tiredness Not Menopause
It’s worth noting that hot flashes and tiredness are not always linked to menopause. Other conditions, such as thyroid disorders or chronic fatigue syndrome, may also cause similar symptoms. Consulting a healthcare provider is essential for identifying the root cause and receiving appropriate treatment.
Building Resilience
It’s essential to acknowledge that coping with hot flashes and fatigue is a journey. Surrounding yourself with a supportive network, whether through friends, family, or online communities, can make a significant difference. Sharing experiences and tips with others who understand your challenges fosters resilience and a sense of empowerment.
Conclusion
Hot flashes and fatigue may feel like an unwelcome intrusion, but with the right approach, they can be managed effectively. By focusing on healthy habits, stress reduction, and open communication with healthcare providers, women can reclaim their energy and improve their quality of life. Embracing this phase with patience and self-care paves the way for a smoother transition into a new chapter of well-being.