Hot flushes, Dizziness and Anxiety - How are They Related ?
November 30, 2024

Understanding the Link Between Anxiety and Hot flushes: A Comprehensive Guide
Hot flushes and anxiety are both common and disruptive experiences that many women face, particularly during menopause and perimenopause. While hot flushes are a well-known symptom of hormonal changes, the connection between anxiety and hot flushes is less often discussed but equally important. Both anxiety and hot flushes can significantly impact daily life, often exacerbating one another, creating a cycle that can feel overwhelming.
This guide explores the relationship between anxiety and hot flushes, shedding light on the science behind it, how they influence each other, and effective strategies to manage both symptoms. From lifestyle changes and therapy options to direct treatments for hot flushes, this compendium offers an in-depth understanding of the connection and ways to manage it.
What Are Hot flushes?
Hot flushes are sudden, intense feelings of warmth, often accompanied by sweating, flushing of the face, and sometimes chills or rapid heartbeat. These symptoms are a hallmark of menopause, specifically during the transition into menopause (perimenopause) when hormonal fluctuations are at their peak. Although hot flushes can affect anyone, they are particularly common in women during their late 40s to early 50s as they experience hormonal changes related to the end of their reproductive years.
The Physiology of Hot flushes
At the core of hot flushes lies the hypothalamus, the part of the brain responsible for regulating body temperature. During menopause, the drop in estrogen levels causes the hypothalamus to become more sensitive to changes in body temperature. When the hypothalamus misinterprets the body’s temperature, it triggers a response that results in a hot flash. This response includes the dilation of blood vessels, which increases blood flow to the skin, leading to the sensation of heat.
While hot flushes are primarily caused by hormonal changes, their severity can be influenced by several other factors such as stress, anxiety, environmental factors, and personal lifestyle habits.
What is Anxiety?
Anxiety is a natural response to stress, characterized by feelings of worry, nervousness, or unease. It is a normal part of life and can be beneficial in certain situations, preparing the body to deal with challenges. However, when anxiety becomes chronic or overwhelming, it can interfere with daily life. During menopause, anxiety is a common issue as women navigate both the physical and emotional challenges of this transitional period.
Anxiety may present itself in many ways, including persistent worry, restlessness, racing thoughts, muscle tension, difficulty concentrating, and sleep disturbances. It is important to recognize that menopause-related anxiety may feel different from general anxiety or other anxiety disorders. Women may find that anxiety during menopause is specifically tied to hormonal fluctuations, shifts in body image, or life changes such as aging, career transitions, or family dynamics.
The Link Between Anxiety and Hot flushes
While hot flushes are generally linked to hormonal changes, anxiety plays a pivotal role in both triggering and intensifying these episodes. Here’s a closer look at the mechanisms behind this connection:
1. Anxiety Triggers Hot flushes
Anxiety activates the body’s sympathetic nervous system, the “fight or flight” response. This leads to the release of stress hormones such as cortisol and adrenaline. These hormones increase heart rate, blood pressure, and overall body temperature, which can mimic the physical symptoms of a hot flash. For many women, the sudden heat or discomfort brought on by anxiety can feel indistinguishable from a hot flash.
Additionally, anxiety often leads to shallow breathing, increased heart rate, and muscle tension, all of which contribute to the sensation of heat. In stressful situations, even women who don’t regularly experience hot flushes might feel the effects of this physiological response, especially during menopausal transition.
2. Hot flushes Trigger Anxiety
On the other hand, the onset of a hot flash can provoke anxiety, especially when the symptoms occur unexpectedly or in public settings. Women may worry about the embarrassment of sweating in front of others or the sudden discomfort that can come with a hot flash. The fear of hot flushes, particularly in social or professional situations, can contribute to heightened anxiety levels, creating a vicious cycle of anxiety and physical discomfort.
3. The Vicious Cycle of Anxiety and Hot flushes
The relationship between anxiety and hot flushes can create a vicious feedback loop. Anxiety can cause hot flushes, and the distress of experiencing a hot flash can, in turn, exacerbate anxiety. This cycle is often difficult to break, as each symptom feeds into the other, making both conditions feel more intense.
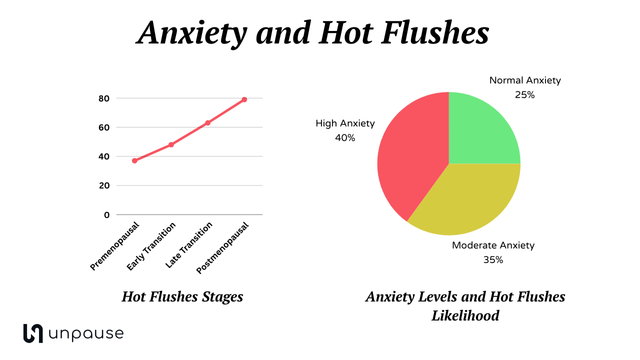
This infographic has been created based on the study published in pmc.ncbi.nlm.nih.gov
Can Anxiety Increase the Frequency of Hot flushes?
Yes, research indicates that anxiety can increase the frequency of hot flushes. A study published in Menopause (2016) highlighted that women who experienced higher levels of anxiety were more likely to report frequent and severe hot flushes. The research concluded that anxiety triggers physical responses that amplify vasomotor symptoms (like hot flushes) and that women with heightened anxiety are at a higher risk of experiencing these symptoms.
Strategies to Manage Anxiety and Hot flushes
Given the interplay between anxiety and hot flushes, effective management involves addressing both conditions simultaneously. Fortunately, there are many strategies and treatments that can help reduce the frequency of hot flushes and manage anxiety levels:
2. Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a form of talk therapy that can be particularly effective in managing both anxiety and hot flushes. CBT helps individuals identify and change negative thought patterns, teaching coping strategies and relaxation techniques. For those experiencing anxiety and hot flushes, CBT can be used to reduce worry about hot flushes and teach calming techniques to prevent them. Studies show that CBT can significantly reduce both anxiety and vasomotor symptoms, making it an effective, non-invasive treatment option.
2. Mindfulness and Meditation
Mindfulness practices such as yoga, deep breathing exercises, and meditation can help reduce both anxiety and hot flushes. These practices encourage relaxation and self-awareness, which can help calm the nervous system and reduce the physical symptoms of anxiety. Mindfulness also fosters acceptance of the body’s natural processes, such as hot flushes, helping women to better manage the emotional responses associated with them.
3. Hormone Replacement Therapy (HRT)
Hormone Replacement Therapy (HRT) is a well-established treatment for alleviating hot flushes and other menopausal symptoms. HRT works by replenishing estrogen levels, helping to stabilize the body's temperature regulation system. While HRT may not directly treat anxiety, it can reduce the frequency and severity of hot flushes, making it easier for women to manage both their physical and emotional symptoms.
4. Non-Hormonal Medications
For women who cannot or prefer not to use hormone therapy, non-hormonal medications such as selective serotonin reuptake inhibitors (SSRIs) or gabapentin may be prescribed to reduce hot flushes. These medications, typically used for anxiety or depression, can have a positive effect on reducing vasomotor symptoms. SSRIs like paroxetine and venlafaxine, for example, have been shown to reduce the frequency and severity of hot flushes.
5. Lifestyle Modifications
- Exercise: Regular physical activity helps reduce stress and anxiety while promoting overall health. Exercise releases endorphins, which are natural mood elevators, and helps regulate body temperature.
- Dietary Changes: Certain foods can exacerbate hot flushes and anxiety. Caffeine, spicy foods, alcohol, and high sugar intake can trigger or worsen hot flushes. Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help stabilize mood and reduce hot flushes.
- Sleep Hygiene: Hot flushes often disrupt sleep, which can increase anxiety. Practicing good sleep hygiene, such as maintaining a consistent bedtime routine, limiting screen time before bed, and using cooling pillows or fans, can improve sleep quality and reduce both anxiety and hot flushes.
6. Social Support
Social support plays a crucial role in managing both anxiety and hot flushes. Talking about the challenges of menopause with friends, family, or support groups can provide emotional relief and reduce feelings of isolation. Online communities, such as forums and social media groups, offer opportunities to connect with others experiencing similar symptoms, providing comfort and shared strategies for coping.
Conclusion
The relationship between anxiety and hot flushes is complex but manageable. The physiological and emotional connections between these two conditions mean that one can exacerbate the other, creating a cycle of discomfort. However, by understanding this connection, women can take proactive steps to manage both symptoms effectively.
Whether through therapies like CBT, medications, mindfulness practices, or lifestyle changes, there are many ways to reduce the impact of hot flushes and anxiety. The key is recognizing that both symptoms are interconnected and addressing them holistically, ultimately leading to a better quality of life during menopause and beyond.